- Call: 1-855-264-2174
Mon to Friday, 8 am – 8 pm (EST) - Email: groupbenefitssolutions@rbc.com
- Visit: Plan Administrator Resources Website
- Mailing Address:
RBC Life Insurance Company
PO Box 1600, 8677 Anchor Drive
Windsor, Ontario, N9A 0B3
Use this guide as a tool to help manage and administer your company’s group benefits program.
Get Started Enrolment/Eligibility Employee Changes Flex Plans Guarantee Standard Issue (GSI) Billing Submit Claims Forms Wellness Spending Account All Sections
Get Started
Use the Get Started overview to register, activate and reset your password within Online Administration.
Tip: If you require assistance, please contact the RBC Insurance Group Benefits Team at 1-855-264-2174.
Your role as a plan administrator of your company’s group benefits plan includes:
- Enrolling or re-enrolling new employees or terminating plan members
- Reporting and updating coverage due to life changing events, i.e. newborns, change in dependents, etc.
- Changing spousal coverage, salaries, division or class
- Validating student eligibility
- Paying premiums
- Keeping accurate and up to date employee records
- Encouraging employee awareness and understanding of their benefits and the resources available
A Wealth of HR Resources for Plan Administrators!
Your RBC Insurance Group Benefits provides free access to our RBC Insurance HR Support Centre, which includes ready-to-use HR policies and templates, up-to-date information on employment standards legislation and more. Access the link from the top menu bar to learn what resources are available to support you as a plan administrators.
Plan Members with Extended Health & Dental benefits will receive an ID Card and will manage their health and dental benefits with our secure Online Insurance. Refer to Quick Start Guide and to Demo.
Plan Members with Extended Health & Dental benefits can manage their health and dental benefits with our mobile app.
As the Plan Administrator you will receive Identification Cards for Plan Members when they are enrolled. Electronic copies are also available for Plan Members via Online Insurance or RBC Insurance My Benefits App. Refer to the ‘How to’ section ‘Print an ID Card’ for detailed instructions.
RBC Insurance is committed to preventing fraudulent activity. Audits on group benefits claims are conducted regularly to help guard against the misuse of plans – both intentional and unintentional.
Fraud increases plan costs for you as the employer which puts coverage at risk. You may end up needing to pay increased premiums or lose certain benefits to cover these higher costs.
Your plan members may receive a claim audit questionnaire and these should be completed promptly, as it helps us protect all of your plan members and their benefit plans from abuse.
Access our new Demo Hub to understand how to submit a claim, check your benefits eligibility and other plan features available online.
Tip: If your email changes at any time, be sure to update your profile with your new email address.
Enrolment and Eligibility
You are responsible for managing the enrollment or re-enrollment process. Having new employees enrolled at the start of their employment should be an integral part of your on-boarding even though insurance coverage may not become effective until a future date. The following processes can help you administer your group benefits plan.
Prior to enrolling an employee confirm their eligibility as follows:
- Is employee a resident of Canada and are they covered by the provincial health care plan? If no, they are not eligible for coverage unless they have a valid work permit in effect and have Provincial Health Care coverage or an equivalent health insurance policy from an insurer that provides for emergency medical coverage in the event of an injury or sickness.
- Is employee in a covered eligible class as defined in group policy? If no, they may not be eligible for coverage.
- Is employee a permanent employee and working the minimum number of hours per week as defined in group policy? If no, they may not be eligible for coverage.
- Is the employee’s salary aligned with the definition of earnings as defined in the group policy? If not, be sure to verify prior to enrolling.
- Please note that plan member’s gender is a required field and is only used for the purposes of determining rates. RBC Insurance will not communicate with the plan member in any way that denotes gender. When entering this information, please use the gender that the plan member self-identifies with: male (M); female (F); or other (U).
To help you capture required information to register your employee first have your employee complete the Group Enrollment Form and then sign into Online Administration to enrol your employee. Keep the Group Enrollment Form original on file. Refer to the ‘How to’ section ‘Add a plan member’ for detailed instructions.
Tip: To avoid a request for Evidence of Insurability, it is imperative that all eligible employees be enrolled within 61 days following the completion of an employee Waiting Period, or the date he/she becomes eligible for coverage.
Tip: If your company does not have a formal on-boarding process, check out the “New Hire Checklist” template on our RBC Insurance HR Support Centre which can be customized to support a comfortable on-boarding process for new hires.
Refer to your group policy for your plans waiting period as it must be adhered to. Eligible employees who are hired after the effective date of your group policy are eligible for coverage following the waiting period. When enrolling using Online Administration the tool will automatically apply any required waiting periods.
To waive the waiting period of a new hire one of the following conditions must apply:
- It is a condition of their employment
- The employee has moved from part-time or contract to full-time status and has satisfied the waiting period during their period of employment
- The employee earns more than $50,000 annually
Enroll the employee using “Add A Plan Member”, confirm you wish to waive the waiting period. Acknowledge that the criteria is met and select “‘Next” to proceeed.
- If you select “YES” to waive a waiting period, you will receive a drop down with the confirmation of allowances for waiving a waiting period.
- If the plan member does not meet the criteria, you can change the response to NO and the waiting period will apply.
- If you confirm to the terms for Waiving the Waiting period, Input “NEXT” and the coverage will begin on the date of hire.
Participation requirements are defined in your Group Insurance Contract. Participation is at the plan level and not at the benefit level. An employee must enroll for all benefits with the exception of extended health and dental. Extended health and dental coverage can only be waived for employees and/or their dependents when they have coverage through their spouse or partner’s benefit plan. If the spouse or partner’s coverage subsequently terminates, the employee and/or dependents may enroll under this plan without penalty, within 61 days of the termination of the spouse/partner’s plan. Refer to the ‘How to’ section ‘Reinstating Waived Coverage’ for detailed instructions.
If an employee refuses coverage, please have the employee complete a Refusal of Coverage Form and email to admin@groupinsurance.rbc.com and keep the original form on hand. If application for coverage that was previously refused by the employee is made, an Evidence of Insurability Form must be completed and submitted for review.
The Evidence of Insurability Form must be completed in the following situations:
- When an employee or dependent is a Late Entrant
- When an employee applies for a coverage amount above any no-evidence maximum as defined in your group insurance policy
- When an employee or dependent is re-applying for coverage that was previously cancelled or declined
- When an employee or dependent previously refused coverage under this policy and is subsequently applying
- When an employee or dependent applies for Group Optional Term Life coverage
The employee must complete the Evidence of Insurability Form and email to MedicalUnderwritingSupport@rbc.com. If additional medical information is required, the applicant or the applicant’s physician will be notified directly. We will pay the cost of obtaining this information, except in the case of a Late Entrant (i.e. an employee or dependent who applies for coverage more than 61 days after becoming eligible). In this case, the cost is at the employee’s own expense. You will receive correspondence about our decision, with a duplicate copy enclosed for the applicant. The duplicate copy outlining our decision should be provided to the employee.
If approved, the effective date of coverage will be outlined in the approval letter. The coverage approved will be reflected within the next two billing cycles.
Tip: If an Evidence of Insurability form is requested the employee will show as ‘not eligible’ on the bill until the Evidence of Insurability form is approved.
Rehired within 6 months:
- If employee returns to work within 6 months, you can automatically waive any waiting period and re-enroll the employee. The employee must be reinstated within 61 days of being rehired. To do this simply email admin@groupinsurance.rbc.com or use the ‘contact us’ feature with your groups policy number, name of the returning employee, the date the employee returned to work and the effective date of coverage.
Rehired after 6+ months:
- If the employee returns to full-time work more than six months after employment termination, the employee is considered a new employee and the waiting period won’t be waived; the usual enrolment procedures are followed. Have the employee complete the Group Enrollment Form and then sign into Online Administration to enroll your employee. Keep the original Group Enrollment Form on file. Refer to the ‘How to’ section ‘Add a plan member’ for detailed instructions.
Rehired after maternity/parental leave or layoff:
- You can waive the waiting period if an employee returns to work on a full-time basis after the end of a statutory maternity/parental leave or a layoff if the employee elected to discontinue coverage during the maternity/parental leave of absence. The employee must be reinstated within 61 days of returning. To reenroll the returning employee, email admin@groupinsurance.rbc.com with your policy number, name of the returning employee’s name, the date the employee returned to work and the effective date of coverage.
Employees on Work Assignment Outside of Canada
- Business travel for 12 months or less to a country not considered “High Risk” below is permitted.
- Business travel to any country exceeding 12 months requires approval.
- Business travel for any length of time to a “High Risk” or “Country of Concern” requires approval.
- An Out of Country Business Travel form must be completed when approval is required as outlined above.
“High Risk” Countries or “Countries of Concern” are generally defined as ones where the Government of Canada has a “avoid all travel” advisory in effect. Our current countries of concern are:
- Afghanistan
- Belarus
- Burkina Faso
- Burundi
- Central African Republic
- Chad
- Democratic Republic of the Congo
- Eritrea
- Ethiopia
- Haiti
- Iraq
- Iran
- Lebanon
- Libya
- Mali
- Mauritania
- Myanmar (Burma)
- Niger
- Nigeria
- North Korea
- Russia
- South Sudan
- Sudan
- Syria
- Ukraine
- Venezuela
- Yemen
As part of strengthening French language requirements, the Quebec government has introduced Bill 96, effective June 1, 2023. Bill 96 requires businesses to respect their Quebec residing clients’ right to be informed and served in French.
To comply with the Bill 96 regulations, RBC Insurance will be providing the ‘Plan member booklets/ certificates’ in both English and French to plan members residing in Quebec. Non-Quebec residing plan sponsors with Quebec based employees can reach out to RBC Insurance Sales and Service teams to request French booklets.
When speaking to clients residing in Quebec, remember to:
- Present applications and all other policy documents in French first, even if their preferred language is English.
- Delete any previous versions of the applicable paper forms and the online enrollment templates. We strongly encourage you to use the new updated versions dated June 2023 and onward, as using an incorrect version may result in the application being rejected.
Employee Changes
As the Plan Administrator it is important you keep all plan member changes up to date.
Examples of changes include:
- Change in plan members’ personal information such as name, language, adding or removing dependents or changing family status from Single to Couple or Family. Example; Changes due to marriage, qualifying a common-law partner, legal separation or divorce, birth or adoption of a child
- Change of division, class or location
- Change of role, salary or number of hours worked
To help you capture required information to register any changes first have your employee complete the Group Benefits Change Form and use Online Administration and refer to the ‘How to’ section ‘Modify or Correct an Error to Existing Information’ for detailed instructions.
All changes must be reported using Online Administration within 31 days of the effective date of the change. Any changes outside of 1 month prior and 1 month after the change cannot be completed using Online Administration and will require you to contact our administration team to make the change.
Certain types of Plan Member Changes can be processed using our Mass Transaction functionality allowing real time processing of these requests. The types of changes that can be processed as a mass transaction include:
- Salary Updates
- Billing Division Changes
- Class Changes
- Cost Centre Changes
- Terminations
- Reinstatements
Refer to the ‘How To’ section, ‘Mass Transactions’ for detailed instructions.
Tip: Alternatively, you can upload a spreadsheet of Plan Member Changes via Online Administration to be processed by our Group Administration team.
If a plan member has a dependent who is a full time student at an accredited college or university and has attained the age of 21, but is under age of 26, enrolment in that college or university must be confirmed on an annual basis. At the beginning of each school year, we will send you a list of plan members and their dependents who are between the ages of 21 and 26. You will have 60 days to contact your plan members to validate the accuracy of the dependent information and report back to RBC Insurance.
Confirming the accuracy of this information ensures eligible dependents are continuously covered for their health and dental benefits through to September next year.
Tip: As the plan administrator you can add or remove dependents using Online Administration and refer to the ‘How to’ section ‘Add a dependent’ or ‘Terminate a dependent’ for detailed instructions. You will be able to select dependent, special needs dependent or spouse.
Tip: Plan Members whose children are transitioning to post-secondary education, may be interested to know that their Employee Assistance Program (EAP) offers support with college selection and application process, understanding funding options and counselling for any emotional issues experienced during this transition. Let them know that support is available.
To change a beneficiary designation, where allowed by law, have the plan member complete the Beneficiary Designation Form and retain the original form for your records.
You can make the necessary change by signing in to Online Administration and update the plan members’ beneficiary. Use Online Administration and refer to the ‘How to’ section ‘Modify or Correct an Error to Existing Information’ for detailed instructions.
In the unfortunate event of a plan member’s death, coverage may continue for the eligible covered dependents until the earliest of the following dates:
- 24 months after the date of death;
- The date the covered person would no longer be considered a dependent under the plan if your plan member were still alive; or
- The date the benefit plan under which the dependent is covered terminates.
Use Online Administration to update the plan member’s death and add the surviving spouse benefits. Once the surviving spouse is added, an ID card and letter will be mailed to you. This letter advises the surviving spouse on how to register for the Online Benefit Solutions Service.
Tip: Let the surviving spouse know that they and their dependents have access to qualified counsellors through the WLEAP that can provide support during this difficult time.
Terminations for Plan Members who are no longer covered under the plan must be processed quickly so that additional claims are not incurred. Terminate employees by signing in to Online Administration within 14 days of the termination. Refer to the ‘How to’ Feature ‘Terminate a plan member’ for detailed instructions.
Tip: If you need some guidance regarding what steps should be taken when an employee is terminated, refer to the “Termination Checklist” template in your RBC Insurance HR Support Centre.
Please review the complete details of the Employment Insurance Act and your provincial Employment Standards Act for maternity/parental leave provisions. Coverage can continue while plan members are on maternity leave as long as premiums are paid up to the maximum period allowable under the maternity provisions of the Employment Insurance Act and Employment Standards Act, unless the employee gives the employer written notice that the employee does not intend to continue to participate in the plan.
If the plan member elects to discontinue coverage, all coverage will cease. If the plan member elects to opt out of coverage, have the plan member complete the Maternity/Parental Leave of Absence – Opting out of coverage form and retain the original form for your records. Sign in to Online Administration to terminate coverage. Refer to the ‘How to’ Feature ‘Terminate a plan member’ for detailed instructions.
Tip: For up-to-date information on employment standards legislation reference RBC Insurance HR Support Centre and access the link from Online Administration. Before an employee leaves on Maternity/Parental leave let them know that their EAP program is there to support them with valuable resources on topics such as pre-and post-natal health, child development, assistance finding child care and counselling services if required.
Terminated employees may be eligible to convert their coverage, as outlined in the Group Policy and as may be required by law. Terminated employees should contact RBC Group Benefit Solutions Service Team at groupbenefitsolutions@rbc.com or by calling 1-855-264-2174 for a quote immediately. Applications can be retrieved under service forms and must be received by RBC Insurance within 31 days following the employee termination.
Tip: Plan Members can sign in to Online Insurance service and update their personal banking information and home address for claims processing.
Flex Plans
Group Benefit Solutions Flex Plans plan members will have the option to select their extended health and dental Benefits.
To help you capture the required information to register your employee, first have your employee complete the Group Enrollment Form then sign into Online Administration to enrol your employee. If an employee does not select a module the employee should be placed in the plan option level with the lowest level of coverage. Keep the Group Enrollment Form original on file. Refer to the ‘How to’ section ‘Add a plan member’ for detailed instructions.
If a life event occurs, as outlined below, the employee may change classes within 60 days of the life event.
To help you capture the required information to register any changes, first have your employee complete the Group Benefits Change Form. Refer to the ‘How to’ section ‘Modify or Correct an Error to Existing Information’ for detailed instructions
All changes must be reported using Online Administration within 60 days of the life event.
A Life event constitutes one of the following:
Adding a Dependant
- Marriage
- Qualifying a common-law partner
- Birth of a child
- Adoption of a child
- Accepting legal guardianship of a child
Removing a Dependent
- Divorce
- Legal separation
- Disqualifying a spouse/partner
- Death of a spouse/partner or child
Change in Coverage
- Loss or gain of spouse’s coverage
Tip: Life events can sometimes be stressful, let your plan members know that the EAP program provides access to qualified counsellors and valuable resources should they need support.
Upon your selection date use your Benefit Selection Sheet and ensure plan members are alerted of the selection period and make their choice by the selection deadline. For those employees who wish to make a change, we recommend they complete Benefit Selection Sheet to make their selection.
To make the changes sign into Online Administration or once all employees have made their selection sign into Online Administration WebShield Stats and download the census report. On the census report, note any employees who have made a class change.
Email the census report to admin@groupinsurance.rbc.com for the changes to occur. Note - any benefit selection changes will take effect on the benefit selection end date.
Guarantee Standard Issue (GSI)
Refer to this section if your group benefit plan includes Guaranteed Standard Issue (GSI) coverage.
Prior to enrolling an employee, confirm their eligibility. Refer to this table for enrolling new employees in a GSI class.
Is the employee a Canadian Citizen, or a Permanent Resident (landed immigrant)? If the employee answers ‘no’ to this question in the enrollment tool, it will inform them that a Foreign Contract Questionnaire is required. The employee may ignore this and proceed with the application since this questionnaire has been discontinued. Their application will continue to be directed to the GSI Underwriting area who will proceed to include a Least Restrictive travel exclusion amendment to their policy contract. In the event the member completes the FCQ after April 27th, Underwriting will disregard and proceed with a least restrictive travel amendment.
GSI Enrolment:
| If... | And... | And... | Then... |
|---|---|---|---|
| the employee is eligible for the GSI Program | GSI Online Application | has been enrolled with the Online Administration | 48 hours after you have enrolled the employee email the personalized GSI Online Application link to your employee to apply using the tool. |
| the employee is eligible for the GSI Program | Paper application | has been enrolled with the Online Administration | forward a copy of the completed combined GROUP ENROLMENT AND GUARANTEE STANDARD ISSUE® (GSI) APPLICATION FORM: Email: gsiapplications@rbc.com |
| the employee is eligible for the GSI program with no group benefits | GSI Online Application | no action required | 48 hours after you have enrolled the employee email the personalized GSI Online Application link to your employee to apply using the tool. |
| the employee is eligible for the GSI program with no group benefits | Paper application | no action required | forward a copy of the completed combined GROUP ENROLMENT AND GUARANTEE STANDARD ISSUE® (GSI) APPLICATION FORM: Email: gsiapplications@rbc.com |
Tip: To avoid a request for Evidence of Insurability, it is imperative that all eligible employees be enrolled within 61 days following the completion of an employee Waiting Period, or the date he/she becomes eligible for coverage
Employees are eligible to continue their GSI policy as a standalone individual policy. Once you terminate a plan member using Online Administration, RBC will send a letter to the prior employee and outline the payment options (monthly bank withdrawal via monthly preauthorized chequing or annual direct billing) and the premium amount due. You should inform the terminating employee that any premium discount currently on the policy is transferable to an individually paid policy.
In addition, if the insured were to leave the GSI group that is composite billed, they can maintain their policy but they will need to start paying the premium shown in their individual policy schedule.
Tip: Once an employee is terminated, terminate the employee using Online Administration within 14 days. Employees will only have a limited amount of time to conserve the policy after terminating employment.
If an insured's smoking status changes, the insured may be eligible for non-smoking rates. The insured must complete the Smoking Declaration and email to gsisalessupport@rbc.com for consideration.
Policies under your GSI Program are individual policies. Therefore, in order for the policy to remain in force, the premiums must continue to be paid. If the layoff or leave of absence is temporary, the employee should continue to pay their premiums. If the employee is unable to pay the premiums, the coverage will lapse and it will be necessary for the employee to re-apply for coverage upon return to work. As a result, there may be a change in premiums.
If the layoff is permanent, use Online Administration to terminate the employee within 14 days. If you wish to have the policy removed from your bill, please email admin@groupinsurance.rbc.com. If the policy can be maintained independently, we will contact the employee regarding the options that are available. If you wish to reinstate the employee and the employee did not maintain their GSI policy individually while laid off, they must reapply for a new GSI policy.
Policies under your GSI Program are individual policies. Therefore, coverage under the policy may continue while the employee is on maternity/parental leave. In order to maintain the coverage, the premiums must continue to be paid. If the premiums are employee paid, the employee may elect to pay the premiums on their own during their maternity/parental leave, or pre-pay the premiums through your Company and remain part of your Plan.
If the premiums are company paid, they must continue to be remitted in order for the coverage to remain in force.
If the premium payments are not maintained during the maternity/parental leave, the coverage will lapse due to nonpayment. The employee would then be required to re-apply for coverage upon return to work. As a result, there may be an increase in premiums.
It is not necessary to report an employee on maternity/parental leave to RBC Insurance unless premium payments will be interrupted. If the plan member elects to opt out of coverage, have the plan member complete the Maternity/Parental Leave of Absence – Opting out of coverage form and retain this form for your records.
Sign in to Online Administration to terminate coverage. Refer to the ‘How to’ section ‘Terminate a plan member’ for detailed instructions
A composite rate is an average premium rate based on all of the coverage provided under a collection of individual policies. It can include an adjustment factor to consider changes in the composition of policies throughout the year to minimize changes in the billed premium. Composite billing is a method of premium collection and payment for employee-funded policies where an employer will collect an amount from each employee that is determined by multiplying the employee’s coverage amount by the composite rate. The employer will combine the collected amounts and use them to pay the premiums due under the policies. The composite rate is recalculated at each renewal date for the Plan, and is also recalculated when the premiums collected are insufficient to pay the premiums required by RBC Insurance or if the employer adds a division that will be covered under the composite rate.
What Are the Composite Rate Guidelines?
- RBC Insurance sets guidelines regarding the calculation of composite rates. These guidelines are included in the Administrative Agreement if the Plan Administrator or TPA is calculating the composite rate.
- A “class” means a subset of insureds who share distinct occupational characteristics, such as job level or location, and whose policies are included for the purpose of determining a composite rate applicable to that subset.
- The administrator and employer will determine class structure, and the composite rate for that class is determined by adding all of the individual GSI premiums within the classes and dividing that amount by the total individual GSI coverage within the classes.
- An adjustment margin may be added to reduce the chance premium changes are needed during the year. Maximum margins are set based on the number of policies in the class. Three allowed methods of dealing with smoker premium differences are also provided.
If the Plan Administrator or TPA is calculating the composite rate, use of a trust account is required to hold premiums in excess of the amount required by RBC Insurance. The Administration Agreement describes the maximum amounts and usage of trust account funds. Funds may only be used to reduce future composite rates for members of the composite rate class where the excess premium was generated.
Composite Rate Table
Plan Administrator/TPA Calculates the Composite Rate
A spreadsheet has been provided to calculate the composite rate.
- Administrators may continue to use their own tools and methods to calculate the composite rate if that method is in accordance with RBC guidelines.
- The calculation can only consider individual GSI premiums and coverage. No other coverage (such as group LTD) can be considered.
- Information/attestation will be provided to RBC Insurance to confirm that calculations and administration are in accordance with the Administrative Agreement before GSI offers are renewed.
- Information on the trust account and the composite rates charged will be required.
- Pay RBC statements as billed.
RBC Insurance Calculates the Composite Rate
- RBC Insurance will determine the composite rate based on member census data.
- At renewal, the composite rate is recalculated for the Plan, and is also recalculated when the premiums collected are insufficient to pay the premiums required by RBC Insurance or if the employer adds a division that will be covered under the composite rate.
- No attestation is required on the part of the administrator or the client.
- Pay RBC statements as billed.
If the premium payor for the policy is the employer or a third party, it is necessary to have an employee acknowledge this in writing using the combined Group Enrollment and Guarantee Standard Issue (GSI) Program Application Form for GSI classes or the Group Enrollment Form Group-only classes. This allows you as the employer or TPA to exercise certain policy rights associated with the payment of premiums, and it allows RBC Insurance to:
- Receive and accept premium payments from the employer/TPA,
- Pay any refund premiums to the employer/TPA
- Send any premium notices or premium lapse notices to the employer/TPA
The policy owner still maintains ownership rights and is entitled to receive any benefits that may become due. Please contact RBC Insurance Customer Service for further information.
Billing
Billing Statements are available each month in PDF or Excel format using Online Administration. When your billing is posted to the site, you will receive an email notification with this subject line: “Your bill has been posted to the site”. All premiums must be paid by the due date in accordance with your group policy to ensure continuing coverage and uninterrupted claims service. Non-payment of premiums will result in policies lapsing, and reinstatement will be subject to RBC Insurance reinstatement rules.
The Self Admin Invoice statement will assist you in calculating the premium due for your group insurance plan. This statement must be completed each billing period and coincide with your payment remittance. Refer to the “How to” section “Remit Self Admin Invoice” for detailed instructions.
Tip: Blank fields will be rejected. If a field is not applicable, simply enter a zero (0) in that field. If the net premium submitted varies significantly from the previous billing period, you will be required to provide a reason for the difference. If a correction to any of the submitted date is required, click Return to Data Entry. Otherwise, click the Approve button to complete the Self Admin Invoice submission.
If the employee is required to contribute towards the cost of the coverage, payroll deductions should begin as of the first of the month following or coinciding with the Effective Date of insurance. Each month’s billing will provide you with details identifying the employee’s benefits and cost breakdown for payroll and tax calculations.
- Premiums for employee changes are not pro-rated to the day.
- Below you will find examples outlining when premium is payable for a newly added or terminated employee based on their eligibility date.
Adding an Eligible Employee:
- Once an employee is eligible, they may be added to the plan. Coverage is in force on the date they become eligible.
- Premium for the newly added employee is payable on the next monthly premium due date.
Adding Eligible Employee Example:
| Adding Eligible Employee (after any applicable waiting period) - New Hire | Coverage Effective Date | Premiums Due Date |
|---|---|---|
| March 1st | March 1st | March 1st |
| March 15th | March 15th | April 1st |
| March 22nd | March 22nd | April 1st |
| April 3rd | April 3rd | May 1st |
Terminating an Eligible Employee:
- Coverage is terminated effective on the employee’s last day of active employment at 11:59pm.
- While coverage ends on the last day of active employment at 11:59pm, premiums remain payable up to the next monthly premium due date.
Terminating an Eligible Employee Example:
| Terminating an Eligible Employee: (Last day of Active Work) | Coverage Termination Date (until 11:59 pm) | System Termination (Date displayed on the system) | Premiums are Payable Until: |
|---|---|---|---|
| March 31st | March 31st | April 1st | March 31st |
| April 1st | April 1st | April 2nd | April 30th |
| May 8th | May 8th | May 9th | May 31st |
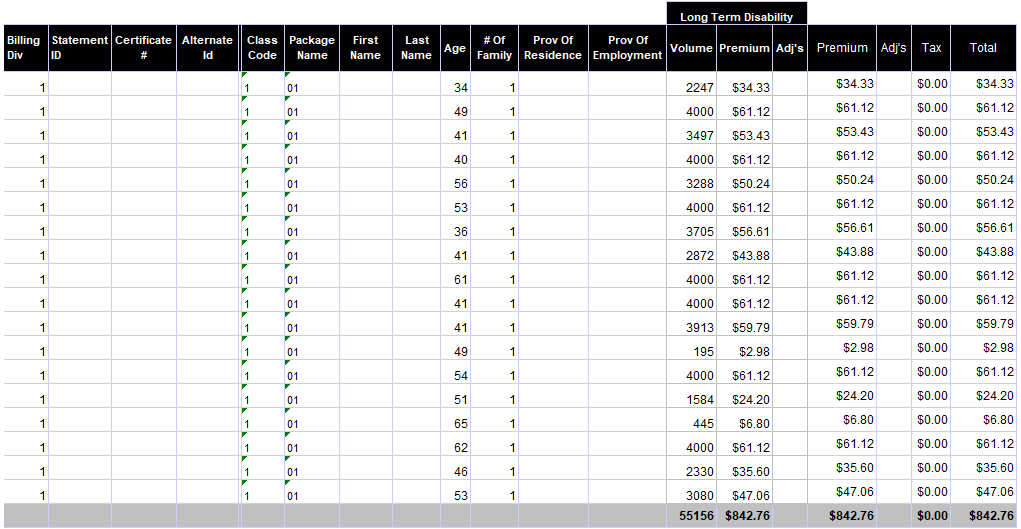
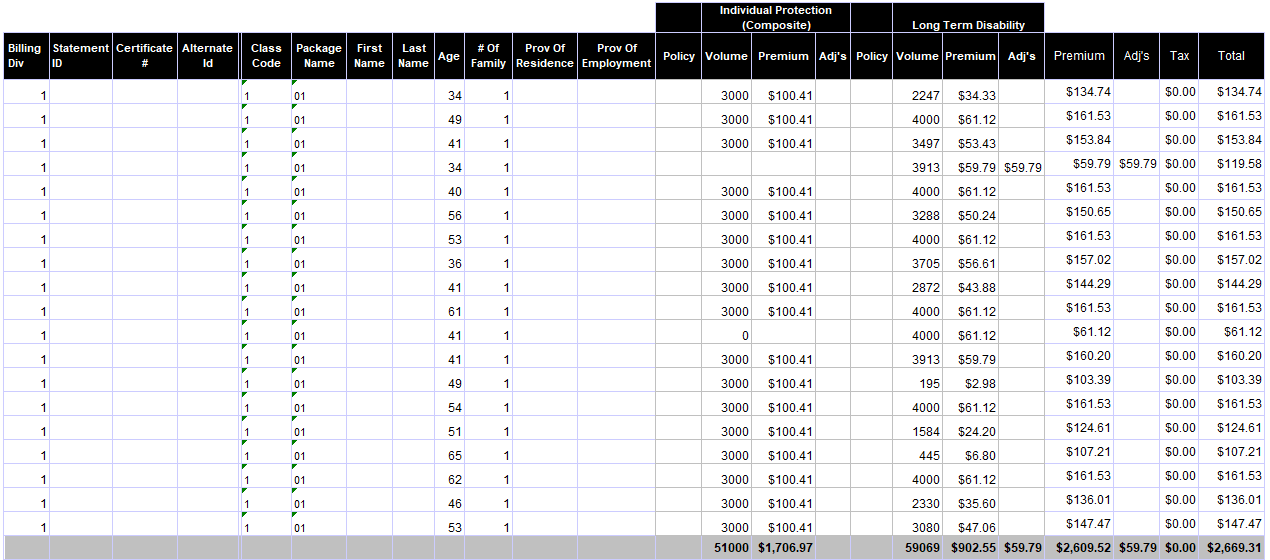
Your billing statement is comprised of 4 parts. To help you understand your billing statement, select the section you require assistance with:
1: Billing Summary and remittance advices: This page summarizes what you owe, clearly showing balance forward, payments received, new charges and total premium. It includes a summarized accounting and tear off remittance statement.
2: Billing Details: This page explains the breakdown and total monthly billing including premium charges, payments and adjustments entered since your last billing was produced. This section details the premium charges by benefit.
3: Change Detail Report: This section shows a consolidated summary of group level changes and a summary of Plan Member changes in one convenient spot.
4: Plan Member Premium Report: This section lists all plan members included in the billing month.
Tip: Billing data is also available via WebShield Stats in a monthy EXCEL report that can be downloaded as required.
RBC Insurance billing system has a standard statement template, but allows the ability to choose additional details to be displayed. If you would like to change any of the defaults please email admin@groupinsurance.rbc.com or call the RBC Insurance Customer Service at 1-855-264-2174 and choose the prompt for billing. We will gladly help you set up one of these options.
- Plan Member Display: The default is for Plan Members to appear on your statement in alphabetical order with the following standard fields: Name, Certificate Number, Products, Province of Employment, Plan Member Class, # of Family, Age, Coverage, Premium, Premium Adjustment, Tax and Total Premium. If applicable, GSI Policy Number is included. You have the option to have the following fields displayed or removed upon request: Age can be removed, Alternate ID or Cost Centre can be added.
- Statement Delivery Options: Our standard delivery option is for online statements via RBC Insurance Online Administration.
At RBC Insurance we have four payment methods available:
- Pre-Authorized Payment: Use pre-authorized payment debiting on the 8th of each month. Complete the Group Benefit Solutions Pre-Authorized Debit Arrangement and email to admin@groupinsurance.rbc.com.
-
Electronic Funds Transfer (EFT) or Wire Transfer: Please ensure to provide the applicable policy number for which the payment is being made when requesting the wire transfer. Please note that all wire payments must be made payable to RBC Life Insurance Company and must be made IN CANADIAN FUNDS. You will need to ensure that your bank also has the appropriate Bank Number, Transit and Account Number, when transferring premium to the RBC Royal Bank. All Wire Transfers must now be made payable to: RBC Life Insurance Company. Initiate the wire transfer by contacting your bank with all of our bank information.BANK: Royal Bank of Canada, Main Branch – Toronto, 200 Bay Street, Main Floor, Toronto, ON M5J 2J5
- ACCOUNT: 1164516
- TRANSIT: 00002
- BANK: 003
- no SWIFT CODE required
Email the following information to advise us when you have transferred a payment to admin@groupinsurance.rbc.com:- Date & Amount of Wire Transfer
- Wire Transfer details such as amount being paid per division
- Policyholder Name & Policy Number
-
Online Banking: RBC Insurance is set up as a payee with the following financial institutions:
- Royal Bank
- TD/Canada Trust
- Scotiabank
- Bank of Montreal
- CIBC
- National Bank
- Hong Kong Bank (HSBC)
- Alberta Treasury Branches (ATB)
To make a payment via online banking you will need to choose RBC Life Insurance Company - Group as the payee and enter the policy number & division number of your account number. This is critical to ensure money is applied in a timely manner.
This is available for group benefit plans set up for Administrative Services Only (ASO) funding arrangements. With this funding arrangement RBC Insurance will issue a monthly billing. The monthly billings will reflect the actual claims experience processed during a given month, plus administration fees, other charges and applicable taxes. The monthly billings contain the balance as at the end of the prior month, payments received and current charges. Other information, such as detailed calculations, claims by province, contact information and the GST/HST amount contained within the claims amount is disclosed on the billing as well. As these invoices are issued after the fact, i.e. after claims have been processed, the expectation is that the statement amount will be paid upon receipt of the statement. If you have questions about your statement, contact your RBC Insurance Customer Service team at 1-855-264-2174.
Tip: Always pay billing statements as billed. Any employee changes previously reported and not included on the current monthly billing statement will be reflected on the next statement with any appropriate back charge or credit.
Tip: At any time if you require assistance with your billings statement or payment, please call us at 1-855-264-2174.
Claims
This section helps you in regards to making claims and supporting your employees when they need to submit claims under their Group Benefits Plan.
For any claim inquiries, please call 1-855-264-2174 or email as follows:
- For Life, AD&D, Disability or GSI Critical Illness claim inquiries, please email claimservice@rbc.com
- For Group Critical Illness claim inquiries, please email: RBCI_CI_Claims@allstatevoluntary.ca
- For Health & Dental claim inquiries, please email healthanddentalclaims@groupinsurance.rbc.com
In the event of a disability, the AWI/STD/ATP – STD Disability Claim Form must be completed and emailed to intake@rbc.com.
There are 3 statements to be completed:
- Disability Claim Form Client’s Statement;
- Employer/Carrier Statement;
- Attending Physician’s Statement – Short Term Disability Claim.
To avoid any delays in the processing of the Short Term Disability claim, all forms should be completed in full and submitted to intake@rbc.com as soon as possible.
As the employer, please be sure to complete the form to the fullest, and include any supplemental information required such as job description, last pay stub or statement, attendance records etc. Additional information may be requested by us upon review of the claim forms.
In the event of a disability (with or without GSI) or a stand-alone life waiver of premium, the Group Disability Claim Form must be completed in full and submitted to intake@rbc.com.
There are 3 statements to be completed:
- Employee: Group Disability Claim Form – Employee Statement
- Employer: Group Disability Claim Form – Employer Statement
- Physician: Attending Physician Statements – for Disability Claims
The employee may select which form to have completed based on their condition. Otherwise, the General form may be used.
To assist in ensuring minimal or no interruption in pay to your employee, claim forms should be completed at least 8 weeks before the end of the elimination period (i.e. the waiting period before benefits are paid).
As the employer, please be sure to complete the form to the fullest, and include any supplemental information required such as job description, last pay stub or statement, attendance records etc. Additional information may be requested by us upon review of the claim forms.
In the event of a life or accidental death claim, the Group Life/Accidental Death Notice of Claim must be completed and submitted to intake@rbc.com.
There are 3 statements to be completed:
- Employee’s beneficiary: Client’s Statement
- Employer: Employer’s Statement
- Physician: Physician’s Statement – should be submitted for all accidental death claims and for life claims of all insurance amounts.
As the employer, please be sure to include the original group enrolment form with your statement. Additional information may be requested by us upon review of the claim forms.
In the event of a loss of use or dismemberment claim, the Loss of Use/Dismemberment Notice of Claim must be completed in full and submitted to intake@rbc.com.
There are 3 statements to be completed:
- Employee: Client’s/Employee’s Statement
- Employer: Employer’s Statement
- Physician: Attending Physician’s Statement
As the employer, please be sure to include the original group enrolment form with your statement. Additional information may be requested by us upon review of the claim forms.
In the event of a disability the Individual Disability Claim Form must be completed and emailed to intake@rbc.com.
There are 2 statements to be completed:
- Employee: Individual Disability Claim Form – Client’s Statement of Disability; and Broker Direction and Authorization
- Physician: Attending Physician Statement – for Disability Claims. The employee may select which form to have completed based on their condition. Otherwise, the General form may be used.
Claim forms must be completed in full as soon as possible following the date of disability. Additional information may be request by us upon review of the claim forms.
In the event of a critical illness, the Notice of GSI Critical Illness Claim Form must be completed in full and submitted to intake@rbc.com.
There are 2 forms to be completed:
- Employee: Notice of Critical Illness Claim form
- Physician: Attending Physician Statement – for Critical Illness Claims. The employee may select which form to have completed based on their condition.
Additional information or medical documentation may be required.
In the event of a group critical illness claim, the Group Critical Illness Claims Form must be completed and emailed to RBCI_CI_Claims@allstatevoluntary.ca.
NOTE: Please download and save the form to your computer or device. Retrieve and open the saved copy in Adobe Reader to complete and submit it.
Depending on the nature of the claim, a plan member's service provider may be able to submit claims electronically on their behalf.
Plan Members may also submit claims through Online Insurance. By selecting Submit Claim and navigating to the Health/Dental option on the Home Page, plan members will be able to submit a health and dental claim electronically. This is also available through the RBC Insurance My Benefits app on a smartphone.
Please contact Allianz Global Assistance:
Visit:
Call:
- 1-855-603-5571 (in Canada or USA) or
- 1-905-608-8251 (collect from anywhere in the world).
This toll-free call centre is available 24 hours a day, 365 days a year worldwide, and can help to ensure you get the care you need without incurring unnecessary out-of-pocket expenses.
Prior to travelling, plan members are encouraged to review their Employee Benefits Booklet to understand what benefits are covered.
The ID card contains contact information in the event of an emergency.
Employees can retrieve printable travel claim forms.
If required, employees can take the Travel Confirmation of Coverage Letter along with their ID Card when travelling to countries requiring proof of coverage.
If a more detailed Travel Confirmation letter is required plan member can call 1-855-264-2174.
Tip: Prior to seeking medical treatment, it is important that plan members calls the number listed on their ID card as soon as possible. The call centre is available 24 hours a day, 365 days a year worldwide, and can help to ensure they get the care they need without incurring unnecessary out-of-pocket expenses.
Forms
Below is a list of forms as well as quick access to claim forms you or your employees may need.
- Annual Allocation of Health and Wellness Spending Account
- Application for Accident Insurance Conversion
- Appointment of Administrator(s) under the Access Agreement for Plan Sponsor
- Beneficiary Designation Form
- Cost Plus Claim Form
- Criticial Illness - Request to Excercise Portability Privilege
NOTE: Please download and save this form to your computer or device. Retrieve and open the saved copy in Adobe Reader to complete and submit it. - Evidence of Insurability Form
- Group Accident Insurance Conversion Notice ($100,000)
- Group Accident Insurance Conversion Notice ($200,000)
- Group Benefits Solutions Pre-Authorized Debit Agreement
- Group Enrolment Form
- Group Life Insurance Accelerated Benefit Notice of Claim
- Group LTD Conversion Facts
- Life Conversion Application – Group Benefit Solutions
- Maternity/Parental Leave of Absence – Opting Out of Coverage
- Modular Flex Plan Benefit Summary
NOTE: To open this PDF, you will need to copy the PDF link and paste it into the Open File dialogue box in Adobe. - Refusal of Coverage Form – GBS
- Plan Member Change Form
- Request for extension of benefits for a terminated employee
Wellness Spending Accounts
A Wellness Spending Account (WSA) is a personal spending account for plan members that is funded by the plan sponsor. The WSA is a taxable benefit to plan members and the plan sponsor is responsible for all payroll-related taxes and deductions, as well as tax reporting to plan members
The Wellness Spending Account (WSA) can be used to pay for a wide range of items related to wellness, predetermined by the plan sponsor as needed for eligible wellness related expenses, for example: gym membership and equipment, wellness services.
When you are adding a new member under your WSA, you will need to enroll the plan member for benefits and enter in the annual contribution amount as part of the add plan member enrollment process. We cannot pay claims for the plan member or dependents until that information is entered into the Online Administration site, within the Spending Account section for the Plan Member. Refer to the ‘How to’ section, ‘Add Spending Account Contributions’ for detailed instructions.
Annual Allotment
Allotments are made annually based on the amount defined in the Master Application. The full year allotment will be available to the member as of their benefit effective date. If the member’s coverage starts after the benefit year begins, the plan sponsor advises if the credits can be pro-rated based on the number of months remaining in the benefit year.
At the beginning of each benefit year, you must provide us with allotment amounts for all members for the new year – even if the amounts are the same as what was allotted for the previous year. Please be sure to send us annual updates well enough in advance to allow us time to update our records prior to the new benefit year. A delay in submitting update information may result in claims being declined incorrectly.
Changes to allotments
We allow changes to WSA allotments as the result of a life event (e.g. marriage, becoming a parent, loss of spouse’s coverage) or change in employment status (e.g. moving from part-time to fulltime status). The plan sponsor chooses whether the WSA allows changes at the time of a life event or employment status change, or if the member must wait until the next benefit year to make the change. WSA credits cannot be withdrawn from the member’s account once they have been deposited
In combination with a Healthcare Spending Account (HSA)
If a plan sponsor also has an HSA they can set up a WSA such that it shares credits with their HSA. Plan Members would then have the option to allocate credits to either a HSA or WSA at the start of the benefit year. Alternately, the plan sponsor can select to have the WSA cover all HSA eligible expenses.
All WSA claims are to be submitted online using our convenient Online Insurance link opens in new window.
Members are allowed 90 days after the end of the benefit year in which to submit WSA claims for expenses incurred during that prior year. WSA claims are paid to the plan member and there is no assignment of payment to any provider. If plan includes EHC/Dental, reimbursement will ‘mirror’ plan members set up for EHC & Dental (i.e., either by cheque or direct deposit). If auto-coordination is set up, amounts paid out of both the core benefit plan and WSA would go on the same cheque and EOB.
- If your WSA offers no carry-over feature:
Plan members have 90 day period after the end of a benefit year to claim expenses that were incurred during that year, after which any credits remaining in a member’s WSA will be lost. - If your WSA offers Carry Over of expenses feature:
Plan members have 90 day period after the end of a benefit year to claim expenses that were incurred during that year, after which any allotments remaining in a member’s WSA will be lost. However, employees may carry expenses forward from one Benefit Period into the next Benefit Period. - If your WSA has a 12 month Carry Over of Credits:
Plan members have 90- day period after the end of a benefit year to claim expenses that were incurred during that year. If they have unused WSA allotments remaining in their accounts at the end of the benefit year, they can carry them over to use along with their next year’s allotment to pay for next year’s expenses. (Next year’s claims would be paid first from the carried-over allotment, before using the new allotment.) Each year’s allotment can only be carried over for one benefit year. At the end of the second year’s proof of claim period, any carried-over allotments still remaining from the first year will be lost.
Billing in arrears. At the end of each month a separate Wellness Spending Account (WSA) bill is available in Online Administration for the plan sponsor, which includes the cost for all claims paid, plus our administration fee, plus applicable taxes.
How To
- Select Add Plan Member from the home screen, or the left-hand menu bar.
- Choose the Billing Division (if applicable) and enter the Date of Hire.
- Enter Personal information and the Canadian Citizen/Permanent Resident question.
-
Choose the appropriate drop down for Extend Health coverage to and Extend Dental coverage to.
Please Note:
If the plan contains life and disability-based benefits only, then choose single coverage for both health and dental.
If the plan is eligible for dependent life coverage, you must answer “Yes” to the dependent question.
If the plan member would like to opt out of volume-based benefits, then a mandatory opt-out form must be completed and sent to the Administration Department.
Single Coverage: If the plan member has only life and disability, choose single coverage in both the health and dental drop-down lists. (Note: If the plan member has dependent life, you must choose the family option in order to give the plan member dependent life coverage)
Family Coverage: If the plan member has health and dental and eligible dependents, choose Plan Member, spouse, and dependents coverage in the health and dental drop-down lists.
Waived Coverage: If the plan member already has health and/or dental coverage and they want to waive their RBC health and/or dental coverage, choose “Waive Coverage” from the applicable drop-down lists.
-
Confirm if waiving the Waiting Period
Confirm that all conditions are met if waiving the waiting period (if applicable). Select Next.
- Complete Personal, Contact Information, Employment and Earnings sections.
-
Enter Dependent Information (if applicable)
If the dependent is a spouse, provide the appropriate response to the ‘Has other coverage’ question.
- Enter the Health and or Wellness Spending Account contributions (if applicable).
-
Review the information entered for accuracy and then click Submit.
The Plan Member has now been added, and a confirmation page will be generated. A new Plan Member ID number is created and displayed on the plan member record at the top of the page below their name.
At this time, you can enter the Beneficiary information (if applicable), edit any Plan Member sections, as well as Pin the plan member, or Print the ID card.
- Within the Online Administration home page, search for the appropriate Plan Member using the search bar. Alternatively, select Search/Edit Plan Member from the left menu bar.
- Scroll down to the Dependents Information section and select Add Dependent(s).
-
Complete the required fields, including First day of coverage and click Save or Add Another Dependent.
Note:
When adding a spouse with coverage under another plan, answer Yes to ‘Has other coverage?’ by moving the toggle to Yes. Select if the spouse has Single or Family coverage under their own plan.
If any of the dependent(s) are 18 years of age or older, you will be prompted to respond to a question confirming if the Dependent is In School.
- If the new addition of dependents affects the family status (i.e. single to family), you will be required to update the following sections: Employment Information.
- Navigate to the Employment Information section.
- Click on Edit or double click on any field.
- Change the Family Status to Plan Member, Spouse, and Dependents.
- Enter the Effective Date.
- Click on Save.
- Within the Add Plan Member process, navigate to the section Spending Account(s).
- Enter in the Contribution Amount(s) in the specific fields.
- Click Submit.
Please note: If the Plan Member is electing to direct Spending Account Contributions to their RRSP. Please enter $0.00 into the Contribution Amount(s) field.
When dependent management is available, Dependent Events allows you to review any new dependents added to your plan by your plan members, or any reinstatements made by your plan members through the plan member portal.
- Select Dependent Events from the left menu bar.
- Enter the start and end date ranges if needed (dates are automatically defaulted to the last 10 days).
- Click on Search.
- Plan member data and dependent data are shown in the results along with the process date of when the plan member made the change.
- Click on Mass Transactions on the left-hand side menu. This view will display the dashboard of Mass Transaction events Completed or in Progress.
- To see specific details on any previous Mass Transactions, select the appropriate row and click on View.
Create a New Mass Transaction
- Click Create New Mass Transaction.
- Select the Type of Change from the drop down.
- Enter the search criteria such as: Billing Division, Status, Class and click on Search.
- Select the plan members you want from the search results:
- From the hamburger menu, Select all on current page will place a check mark next to each plan member and will display the number of records selected.
- Select all # records will include every plan member across multiple pages and will provide the total number of records selected.
- Click on Unselect all to remove the check mark next to each plan member. Click on Confirm in the pop-up confirmation message.
- Or click on specific plan members. A check mark will show which plan members you have chosen.
- Once you have selected all the plan members needed, select Next.
- Enter the effective date and complete any additional information needed to complete the transaction and select Next.
- Review the information and select Confirm Change. The mass transaction has been submitted and will be processed automatically. Completion of the changes will be monetarily delayed depending on the number of transactions requested.
- Click on View Status to go back to the dashboard to check the progress of the request or click on Make Another Change.
Upload Mass Transaction
- Within the Mass Transactions menu, select Upload Mass Transaction.
- Click on Choose File
- Attach the file to be sent for processing or drag and drop the file.
- Click Upload File.
- Click Complete.
Please Note: When uploading a Mass Transaction through file transfer, it will not be displayed in the dashboard.
- Select 'Search/Edit Plan Member'.
- Search for the appropriate Plan Member.
- Navigate to the section you wish to modify or correct and click on Edit to update the information.
- When the information has been successfully updated, choose the Effective Date and click Save.
- Within the Online Administration home page, search for the appropriate Plan Member using the search bar. Alternatively, select Search/Edit Plan Member from the left menu bar.
- Click on the ID card icon from the right side of the Plan Members Name section.
- The Plan Member ID card will be displayed. Click on Print.
Note: ID cards are automatically generated when you add a plan member, add a dependent, terminate a dependent or change the last name or first name of a plan member or dependent.
If you require a replacement ID Card, please contact your RBC Insurance Administrative Support team.
- Search for the Not Active plan member.
- Click on Reinstate icon on the right side of the Plan Member name section.
- Reinstate all dependents or select specific dependents who will be reinstated with the plan member.
- Enter the Effective Date of the reinstatement.
- Click on Reinstate.
- Confirmation message displays. If you wish to proceed with the reinstatement, click on Confirm. If you do not, click on Cancel.
-
Does the reinstatement change the family status of the plan member? If yes, navigate to the Coverage Info section.
- Click on Edit or double click on any field to open the fields for entry.
- For Health Benefits, change the Coverage Level by selecting from the drop down.
- Enter the Effective Date.
- Click on Save.
-
Navigate to the Employment Information section.
- Click on Edit or double click on any field.
- Change the Family Status.
- Enter the Effective date.
- Click on Save.
Note: The plan admin portal limits retroactive reinstatements to 6 months. For reinstatements beyond 6 months, contact your RBC Insurance Administrative Support team.
- Search for the Active plan member.
- Navigate to the Dependents section.
- Click on the ellipsis (...) beneath the Action column, for the dependent you wish to reinstate and click on Reinstate. A Reinstate Dependent section displays.
- Enter Effective Date.
- Click on Reinstate.
-
Confirmation message displays.
- If you wish to proceed with the reinstatement, click on Confirm.
- If you do not, click on Cancel.
-
Does reinstating this dependent change the family status of the plan member? If yes, navigate to the Coverage Info Section.
- Click on Edit or double click on any field to open the fields for entry.
- For Health Benefits, change the Coverage Level by selecting from the drop-down menu.
- For Life and Disability benefits, change the Coverage Level by selecting from the values.
- Enter the Effective Date.
- Click on Save.
-
Navigate to the Employment Information section.
- Click on Edit or double click on any field.
- Change the Family Status.
- Enter the Effective date
- Click on Save.
- On the left menu tab, select ‘Self Admin Invoices’.
- Search for an invoice for the earliest billing period that has a status of ‘Remittance Required’. (Note: if more than one outstanding invoice exists, please complete the earliest outstanding invoice first.)
- Click on Complete Invoice for the corresponding invoice.
- Enter all product and tax details for the billing period and then click Submit. (Note: any entered data will be lost if ‘Cancel’ is selected)
- If the net premium submitted varies significantly from the net premium for the previous period, you will be required to provide a Reason for the difference.
- If a correction to any of the submitted data is required, click Return to Data Entry and go back to Step 4. Otherwise, click Approve to continue with the submission of premium information for the period.
-
Remittance is now complete; a confirmation page will be generated with one of the following statuses:
- Pending Verification: if the net premium submitted varies significantly from the previous period.
- Approved: if there are no issues with your remittance and your payment has already been applied.
- Payment Pending: if there are no issues with your remittance and your payment has not yet been applied or received.
- Search for the Plan Member.
- Click on the Terminate icon on the right side of the Plan Member name section. A Terminate plan member section displays.
- Enter the first date without coverage in the date field and provide a reason for termination.
- Answer if the plan member is deceased and if they have survivors on the plan.
- Click on Terminate.
-
Confirmation message displays.
- If you wish to proceed with the termination, click on Confirm.
- If you do not, click on Cancel.
Note: The system will only process the termination of a plan member 14 days retroactive to the current date.
Surviving spouse coverage will continue under the existing Plan Member ID number – cheques, ID cards, and correspondence will be issued in the name of the surviving spouse. The deceased plan member’s name will continue to be displayed on the billing.
- Search for the active Plan Member.
- Navigate to the Dependents section.
- Click on the ellipsis (...) beneath the Action Column for the dependent you wish to terminate and click on Terminate. A Terminate dependent card displays.
- Enter the first date without coverage.
- Click on Terminate.
-
Confirmation message displays.
- If you wish to proceed with the termination, click on Confirm.
- If you do not, click on Cancel.
-
Does terminating this dependent change the family status of the Plan member? If yes, navigate to the Coverage Information section.
- Click on Edit or double click on any field to open the fields for entry.
- For Health Benefits, change the Coverage Level by selecting from the drop down.
- Enter the Effective Date.
- Click on Save.
-
Navigate to the Employment Information section.
- Click on Edit or double click on any field.
- Change the Family Status.
- Enter the Effective date.
- Click on Save.
- Select ‘Search/Edit Plan Member.’
- Search for the appropriate Plan Member.
- Navigate to the Employment Information section.
- Click on Edit
- Select the appropriate Billing Division from the Billing Division drop down menu.
- Enter the Effective Date of the change.
- Click Save.
This feature allows you to review all updates and changes made by you within the past seven years. You can search by transaction type, by specific date ranges or pertaining to a specific plan member record. It is a great way to see the history of transactions made over time.
- Click on My Transaction Summary from the left menu bar.
- Enter the search criteria such as, Start and End date ranges, transaction type or Plan Member ID number.
- Click Search. A list of plan member records with the transactions performed are displayed.
- Click on Booklets/Contracts from the left menu bar.
- A listing of Booklets, Contracts and Administrative Letters will be displayed.
- Choose the applicable menu bar and click View to open.
You can easily toggle between English and French Booklets (if applicable.)
- Click on View Billings from the left menu bar.
-
Select the Bill Type you wish to view. (if applicable)
- List Billed/Budgeted ASO
- Claims Based Billing (In arrears)
- Select the Month and Year.
- Click on Search.
- When billings are by billing division, each will display separately. Click on the PDF of the bill to view.
- Within the Add Plan Member section, confirm you wish to waive the waiting period by switching the toggle to Yes. Acknowledge that the criteria are met and select Next to process.
- If you select Yes to waive a waiting period, you will receive a pop up with criteria that must be met.
- If the Plan Member does not meet the criteria, you can change the response to NO and the waiting period will apply.
- If you confirm that the Plan Member meets the criteria for Waiving the Waiting period, choose Next and the coverage will begin on the date of hire.
Human Resources and labour law tools, templates and guidance to help you run your business and save you time.
Overview Employment Agreements Tools, Forms, Checklists & Guides Employment Policies HR/Legal Alerts All Sections
Overview
Providing you access to information that will help your business save time and money.
Get the tools, services and information you need. We know that running a business is not easy, so we want to provide you with access to information that can help support your business.
We’ve partnered with e2r®, a leader in employment/ labour law and human resources support, to bring you the RBC Insurance® HR Support Centre website, which gives you access to:
- FREE ready-to-use HR policies, checklists, and templates
- FREE management guides to navigating a variety of HR topics
- Timely updates regarding human resource practices and employment/labour law

Resources in this section have been provided through e2r®
e2r®, through its seasoned employment/labour lawyers and human resources practitioners, provides employers across Canada with unlimited legal and human resources support including employment agreements, employee handbooks, performance management programs together with unlimited verbal guidance and strategy. To learn more about services and support from e2r®, please visit their website.
Employment Agreements
- Employment agreement – Alberta
- Employment agreement – British Columbia
- Employment agreement – Manitoba
- Employment agreement – New Brunswick
- Employment agreement – Nova Scotia
- Employment agreement – Nunavut
- Employment agreement – NW Territories
- Employment agreement – Ontario
- Employment agreement – PEI
- Employment agreement – Quebec
- Employment agreement – Saskatchewan
- Employment agreement – Newfoundland
- Employment agreement – Yukon
Tip: For more resources related to hiring and on-boarding new employees refer to the “Tools, Forms and Checklist Sections" below.
Tools, Forms & Checklists, Guides
To access this resource: Click on the link and you will be directed to the EAP login page. Enter your user ID and Password: Enter your user ID (rbceng) and Password (rbceng).
Employment Policies
HR/Legal Alerts
Stay connected to the latest developments in employment/labour law and human resources. Follow the link below to the e2r® Alerts page for the most up to date best practices and legislative requirements that will support you in managing your workforce. You can also sign up to receive alerts via email through the link below.
See Alerts or Sign UpWorkplace Wellness Toolkit
54% of plan members have at least one chronic disease/condition diagnosis1
80% of working Canadians report their overall wellbeing would improve if their employer offered a personalized wellness program2
94% of working Canadians are more likely to work for an employer that cares about their overall health and wellbeing2
The best employers know the importance of having programs in place to support the health and well-being of their employees. Not only do employees want and expect their employer to offer wellbeing supports, but evidence suggests that healthier employees are more engaged, have stronger attendance rates, and are more productive. In addition, chronic illness and mental health conditions are on the rise, making it difficult for many employees to bring their best, healthiest selves to work, and challenging employers with increasing claims costs. Providing wellness support is more critical than ever—most importantly for your employees, but also for your business.
Wellness also plays an important role when it comes to attracting and retaining top-level talent. The strongest job candidates have a choice when it comes to finding an employer, and many look for comprehensive wellbeing supports and benefit plans when making a decision. The challenge for employers? Knowing where to start when it comes to creating a compelling workplace wellness strategy. RBC Insurance is here to help.
Let’s begin.
RBC Insurance’s Workplace Wellness Toolkit guides you every step of the way. Here’s what you can expect:
- A framework to assess the wellness needs of your workforce
- Tools to help plan and implement initiatives to address those needs
- Ways to monitor progress
By following the step-by-step instructions in this guide, using the ready-made communication templates and tools and leveraging programs included in your RBC Insurance Group Benefits Plan you can create a wellness strategy customized for your company.
1) 2019 Sanofi Canada Healthcare Survey
2) 2019 Ipsos poll for RBC Insurance
Getting Started
With a few thoughtful steps you can create a culture of wellness where employees thrive. Below is an overview of the key steps.
For detailed guidance on how to implement each step, refer to this Checklist. And remember, no matter what approach you choose for your wellness program—turnkey or something more comprehensive—a range of options are included to help you customize the program to your needs.
Plan Administrator Support and Resources
Your RBC Insurance Client Relationship Specialist is here to support you. Your representative can set up a session to walk you through the checklist and provide an overview of the RBC Insurance Wellness Program, the Employee and Family Assistance program and other services that are available to you. Additional sessions can be arranged to introduce these wellbeing programs to your employees and provide information on how to access them. Contact your representative today to book a time that’s convenient for you.
Ready to create a culture of wellness within your organization? Begin with the Workplace Wellness Checklist now!
Use this checklist to guide the implementation of your wellness strategy, utilizing the resources available to you through your RBC Insurance Group Benefits. By creating a strategic plan, you’ll help your employees bring their best selves to work.
Engage Leadership
Meet with your leadership team to introduce the concept of workplace wellness and get their support.
Why this is important: A successful workplace wellness program starts with a commitment from company leaders. Continued success depends on on-going support, and employees are more likely to engage in wellness programs that are promoted by leadership.
How to make it happen: Need help introducing your leadership to the concept of workplace wellness? We’ve got you covered. Your RBC Insurance Client Relationship Specialist (CRS) can lead or support the conversation. Call today to arrange a convenient time to meet.
Share this short video with your business leaders on the benefits of workplace wellness and the features of the RBC Insurance Wellness Program as a quick introduction to the topic.
Get the Whole Team On Board
Send a clear plan of action with the Employee Communication Template
Why this is important: Getting employees enrolled in the RBC Insurance Wellness Program is essential to the success of your Workplace Wellness Strategy. The RBC Insurance Wellness Program will become an important tool in assessing the needs of your employees and delivering wellness activities and information.
How to make it happen: This communication will be more impactful if it’s sent by a senior leader in your organization. Designate a leader to encourage employees to register so that everyone can participate together. Set a target date for employees to complete registration.
Book an employee information session
Why this is important: Your RBC Insurance Client Relationship Specialist (CRS) can use this opportunity to promote all wellness services available to your employees such as the Wellness Program, Work Life Employee Assistance Program, Teladoc and extended mental health services so that they are aware of all the supports available to them.
How to make it happen: Contact your CRS to book a convenient time for your team to receive a demo. Your representative will facilitate a presentation for employees to ensure they’re ready to begin benefiting from all programs and services.
Go the extra mile when it comes to introducing the programs and services to your employees
- Share this Wellness Program promotional video with employees.
-
Post these brochures in your workplace lunch room, other common areas or distribute them to each employee electronically:
Wellness Program Employee and Family Assistance
Program Teladoc Mental Health Support Services - Introduce these wellbeing supports at your next employee meeting.
- Plan a Wellness Program launch party to coincide with the employee meeting. If budget permits, include healthy snacks and bottled water or hold a raffle for a chance to win a Fitbit, a gym membership, a gift card (which you can purchase at a discount on the wellness platform!) or any other wellness related give-away you think would appeal to your team.
Establish a Baseline
Promote the Total Wellness Assessment (TWA) within the Wellness Platform to your employees.
Why this is important: Completing this assessment will empower your employees to take action by providing them with personal health risk information. You’ll receive valuable, consolidated data about the needs of your employees and their “readiness” to improve their health (for clients with more than 50 employees registered). Note: To maintain employee confidentiality, individual employee data is not visible to the employer.
How to make it happen: With only a few clicks you can send a templated communication to all employees, promoting the Total Wellness Assessment. Refer to the “Promoting Health Assessments” section of the Wellness Program Plan Administrator Guide for more information.
Review your Benefits Plan claims data
Why this is important: Reviewing your Benefits Plan claims data may uncover areas of risk specific to your employee population that can help you target wellness activities to meet the needs of your employees and monitor progress over time.
How to make it happen: Accessing this information is simple:
- Login to the Group Benefit Solutions Online Administration website.
- Click on “Web ShieldStats” on the left menu bar under “Reporting”.
- Select “Reports”, then “Claims” and then “Analysis of Claims by Category”.
- For more information on navigating Web ShieldStats refer to the Web ShieldStats Quick Reference Guide housed on the Group Benefit Solutions Online Administration website
Note: Some reports are only available to employers with more than five employees. If you need help with analysis of the report data, contact your RBC Insurance Client Relationship Specialist.
Complete the Healthy Workplace Assessment
Why this is important: Measuring the current health status of your organizational environment and practices, which are important contributors to employee health, will serve as a baseline for assessing progress over time.
How to make it happen: Complete the Healthy Workplace Assessment template at launch and repeat it at regular intervals (recommended annually) to identify areas of progress and areas that your company may choose to focus on going forward.
Distribute the Wellness Interest Survey to Your Employees
Why this is important: This survey will help you understand what types of wellness programs your employees are interested in and how they prefer to participate. This feedback together with the data collected above are important to the creation of a wellness strategy that is customized to the needs and wants of your employee population. This customization will increase the effectiveness of your efforts to support employee wellbeing.
How to make it happen: Send the Wellness Interest Survey to employees and repeat it at regular intervals (recommended annually). We recommend copying the questions into an automated survey tool, such as Survey Monkey, to protect anonymity and simplify consolidation of feedback. Feel free to customize the survey by adding questions that may be of interest to your organization.
Identify Workplace Wellness Goals
Identify one or more workplace wellness goals
Why this is important: Establishing clear goals will help you focus your efforts and provide a baseline for measuring the progress of your workplace wellness program over time.
How to make it happen: These are intended to be high level. The detailed action plan in Step 6 will include more specific tactics for achieving these goes. Below are some examples of goals:
- Increase employee awareness of existing mental health support programs
- Increase manager knowledge of mental health in the workplace
- Enhance work environment to support physical health
- Provide support for healthy eating
Refer to the Healthy Workplace Assessment for additional suggestions. Results achieved in your first year can provide a benchmark for setting future goals. Once employees are engaged in the program, more targeted goals can be set according to the needs of your employees. For example, goals for year two of the program can be focused on the specific health conditions that contribute to the highest proportion of claims costs and/or the health risks that are most prominent in the employee population according to the Total Wellness Assessment results.
Assess Available Resources
Identify employee capacity to lead / promote wellness activities
Why this is important: When employees participate in planning and promoting activities, it can be a powerful motivator for co-workers to get involved.
How to make it happen: Consider whether someone has the capacity—as little as one hour per week—to plan additional workplace wellness activities that support your organization’s wellness goals.
Want to do more? Consider polling employees to see if any are interested in volunteering for a Wellness Committee to help plan and execute wellness activities and spread the word about the wellbeing support programs. Having someone from management involved in supporting the committee will improve its effectiveness.
Check the budget: is there room to do more?
Why this is important: The more you can do, the stronger your chances of team engagement. Consider whether funding is available for workplace wellness activities.
How to make it happen: Connect with your human resources or budgeting staff to learn about available funds for prioritizing workplace wellness.
Want to do more? Consider whether your company is interested in providing additional incentives/rewards to employees who complete wellness related activities within the RBC Insurance Wellness Program platform, such as challenges, the Total Wellness Assessment and more. This can be facilitated through the wellness platform. RBC Insurance will take care of fulfillment on your behalf, ensuring employees are rewarded the way you want. Refer to the Wellness Rewards Guide for more information.
Create an Action Plan to Support Goals
After you have identified your organizational goals and assessed available resources you can plan specific tactics to achieve those goals. Remember to keep these goals “SMART": specific, measurable, achievable, reasonable, and time bound. If the program is new to your employees, you may want to start with setting moderate targets for program registration and participation and other activities. For example:
- Increase participation in digital wellness program: within 6 months of launch, 50% of employees will have registered for the wellness program.
- Promote one corporate step challenge and one corporate habit challenge over the calendar year and achieve a minimum of X% participation for each.
- Meet with cafeteria/vending machine vendor to discuss increasing healthy food options
- Implement employee stretch break schedule and provide desk-stretch handouts/video links
Consider starting with the activities below already included in your RBC Insurance Group Benefits coverage. Refer to the Wellness Activities Suggestions list for ideas about other activities that you can plan.
Launch a company challenge to motivate employees
Why this is important: Corporate wellness challenges can motivate employees to participate in health-promoting behaviours. They’re designed for group participation, stirring up friendly competition, fostering a culture of wellness, and enabling a colleague support system.
How to make it happen: To get started, choose one or more challenges from the wellness platform that align with the workplace wellness goals you’ve identified. For step by step instructions refer to the “Corporate Challenges” section of the Wellness Program Plan Administrator Guide.
Want to do more? Plan other wellness activities to support the goals identified in Step 4 and address the needs and wants of your employees. Refer to your completed Healthy Workplace Assessment within this toolkit for other ideas about wellness activities that align with your budget.
Promote wellness resources already included with your RBC Insurance Group Benefit coverage
Why this is important: Save time and money by using existing wellness resources.
How to make it happen: Your Group Benefit plan includes valuable programs to support employee health. We recommend that you create a wellness calendar and schedule specific dates (e.g. quarterly) to remind your employees of the valuable programs available to them.
See the Resource List at the end of this guide.
Share RBC Insurance Wellness Communications with your Employees
Why this is important: To support your promotion of employee health, RBC Insurance plans a variety of activities throughout the year such as perks promotions, wellness webinars and communications. These cover a range of topics across the physical, mental and financial pillars of well being that provide valuable information to your employees and highlight the resources available to them through their benefits plan.
How to make it happen: We’ll provide you with ready-made communications to forward along to your employees. Look out for wellness communications from “RBC Insurance National Office”.
Take a Pulse Check Regularly
Access the reporting within the Wellness Program Plan Administrator Panel
Why this is important: Monitoring engagement levels, efficacy, and excitement about your wellness programs will help you respond quickly and make changes as needed.
Revisit the baseline metrics established in Step 3
This should be done at least once per year to see how your organization is progressing against the goals identified in step 4.
Update goals, resources and activities
Determine if your company’s wellness goals should be revised for the coming period, what resources are available and what activities should be planned to support those goals. Revisit steps 3-7 at least once per year.
Implementation Checklist
Implementation Checklist
Download this Implementation Checklist to facilitate discussions with your Leadership Team or Wellness Committee.
Looking for more information or need a little help? Here are a few helpful websites and tools:
Wellness Program Implementation
- Program Brochure
- Video for Plan Administrators and Leadership Team
- Video for Employees
- Implementation Checklist
- Healthy Workplace Assessment
- Wellness Activities Suggestion List
- Employee Communication Template
- Employee Interest Survey
- Wellness Program Rewards Guide
RBC Insurance Digital Wellness Program Platform
- Wellness Platform Guide for Plan Administrators
- Wellness Platform Guide for Plan Members
- RBCI Wellness Program Reporting Platform: Administrator Guide
- RBCI Wellness Program - Sample Report
Other Wellness Resources for Employees
-
Work-Life Employee Assistance Program
Counselling, work-life referrals, free educational materials, nutritional coaching, naturopathic services, health assessments and more.
-
Mental Health Support Services
Show employees you care about their wellbeing and reduce workplace absenteeism due to mental health issues by providing a comprehensive suite of solutions.
-
Maple Virtual Primary Care
With Maple, employees get instant online access to Canadian doctors who can treat issues like colds and flu, infections and more via text message, phone or video.
Plan Sponsor Welcome Guide - Standard
Plan Sponsor Welcome Guide - Premium
Email Templates
-
Teladoc
Confirmation of diagnosis and treatment, referrals to doctors with special expertise, health system navigation
-
Medical Confidence
Provides employees with information and access proper care and treatment throughout their disability claim.
-
Wellness Webinar Series
Enjoy free webinars to support employees and help managers create a supportive workspace.
Your RBC Insurance Client Relationship Specialist (CRS) is here to support you
Your RBC Insurance Client Relationship Specialist (CRS) is here to support you
Your CRS can facilitate a presentation and demo of the RBC Insurance Wellness Program for employees and re-inforce all the wellbeing services available.
Contact your CRS to book a time that’s convenient for you and your organization and they’ll take care of the rest.